
Key Points:
-
Hepatitis C is a viral infection which damages the liver and may cause serious health consequences.
-
No hepatitis C vaccine is available and vaccination against hepatitis A or hepatitis B offers no protection against hepatitis C.
-
Rising trend of hepatitis C among local HIV infected MSM through sexual transmission has been observed in recent years.
-
Sexual transmission probably occurs during unprotected anal intercourse.
-
As with most sexually transmitted infections, hepatitis C is most effectively prevented by consistent and correct use of condom.
-
For those who are injecting drugs, it is extremely important not to share the use of any injecting equipment with others.
|
 |
 |
 What is Hepatitis C? What is Hepatitis C?
Hepatitis C is caused by the Hepatitis C virus (HCV). It is transmitted through contaminated blood or blood products and sometimes the sexual route. After infection, the virus attacks the liver, causing acute and very often chronic infection.
What are the effects of HCV infection?
Most people have no symptoms when they first acquire HCV. They may live with it for many years without even knowing they have been infected. For a minority of patients, symptoms may develop in the acute phase, including fever, fatigue, appetite loss, abdominal pain, nausea, vomiting and even jaundice.
About 80% of infected people would develop chronic liver infection. This may ultimately develop into cirrhosis, liver cancer, and death. |
 How common is Hepatitis C? How common is Hepatitis C?
In Hong Kong, the estimated HCV prevalence in general population is around 0.3%.
Since 2000, there have been increasing overseas reports of acute HCV infections via sexual transmission in men who have sex with men (MSM),especially those who were HIV-positive. Such rising trends have been observed in Europe, Australia, USA and Asia. Locally, the prevalence of HCV in the HIV infected MSM seen at the Department of Health (DH) was found to be 1.3% for the years 2000-2012, which is 4 times that of the general population. In addition, a rising trend of the infection among local HIV infected MSM has been observed in recent years. In 2013, a case series of sexually transmitted HCV infections among HIV infected MSM was reported by DH.
|
 |
How do HIV and HCV affect each other?
A person infected with HIV has a lower level of immunity, making it harder for him to clear HCV. Moreover, co-infection with HIV and HCV can lead to more severe disease and faster progression of hepatitis. This seems to be the case even if you have a high CD4 count.
On the other hand, chronic hepatitis C makes them susceptible to toxicity from HIV treatment and other treatment related to HIV care.
In addition, the presence of HIV infection is thought to increase the susceptibility of getting infected with HCV through sexual contact. |
|
| Who are more likely to get HCV infection?
Hepatitis C is mainly a blood-borne disease. People who share equipment for injecting drug use are most at risk, but sexual transmission does occur.
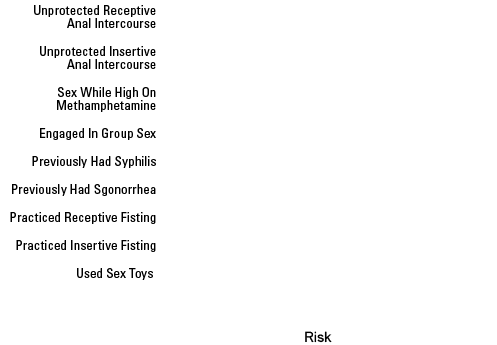
For sexual transmission, unprotected anal sex, having multiple sexual partners, use of recreational drugs and having sexually transmitted infections such as syphilis are known to be associated with HCV infection.
According to a study conducted in the USA, HIV-infected MSM newly infected with HCV were more likely to have risk factors (Chart on the right) |
 |

|
How to prevent HCV?
There is no available vaccine for HCV, but there are effective ways to prevent it.
1. Practice safer sex
- Consistent and correct use of condom, use a new condom for each partner;
- Use adequate amount of lube, do not use lube that may be contaminated with blood;
- Avoid taking drugs or drinking alcohol before or during sex;
- Avoid rough sex which may cause sore and bleeding or burst condom during sex;
- Sex toys like dildos should not be shared. They should be covered with a new condom for each partner. If contaminated by blood, the toys should be cleaned with 1:4 diluted household bleach.
2. Do not share needles. Use disposable needle and injecting equipment each time.
3. Avoid sharing personal care products, including razors, toothbrushes, nail cutters etc.
4. For acupuncture, piercing or tattooing, needles and other equipment should be sterile and/or disposable. |
|
| How is HCV infection diagnosed?
Diagnosis can be made by blood test for antibodies to HCV. People co-infected with HIV and HCV may not produce enough antibodies to be detected, a viral load (PCR) test may be used to confirm the diagnosis.
Regular screening for HCV is recommended for people living with HIV.
HCV antibodies testing services in Hong Kong
| AIDS Concern |
Tel: 2394 6677 |
| C.H.O.I.C.E. |
Tel: 3188 9024 |
|
 |
|
|

|
How to treat HCV infection?
HCV positive persons should be assessed by their doctor for liver disease. Drugs, such as Interferon, Pegylated Interferon and Ribavirin can be used to treat the infection. In addition, newer agents like protease inhibitors are becoming more available for treatment of HCV infection.
Treatment should take into consideration of severity of disease, contraindications, and likelihood of successful response. However, the treatment success rate in HIV infected patients may be limited as compared with monoinfection.
If you suspect you might have HCV infection, please consult your doctor as early as possible. |
| Hepatitis A, B & C at a glance |
| |
Hepatitis A |
Hepatitis B |
Hepatitis C |
| Progression |
|
-
can lead to acute hepatitis and followed by chronic liver damage, including cirrhosis and liver cancer;
-
Approximately 5-10% of infected adults are unable to clear the virus and becomes chronic carriers.
|
-
can lead to acute hepatitis and followed by chronic liver damage, including cirrhosis and liver cancer;
-
Approximately 80% of acute infections do not clear the virus and chronic infections ensue.
|
| Signs and Symptoms |
-
the majority of patients do not have symptoms;
-
flu-like symptoms: fever, fatigue, muscle pain, headache, loss of appetite, nausea and diarrhea. As the condition worsens, jaundice (your skin and white of the eye turn yellow) will occur.
|
| Ways of Contracting |
-
mostly transmitted through contaminated water or food (especially shellfish like oysters, clams, etc.);
-
sexual contact with infected person's stool even in tiny amounts.
|
-
mostly transmitted through mother to child transmission
-
unprotected sexual contact (anal sex, fellatio, etc.);
-
sharing injecting equipment.
|
-
mostly by sharing injecting equipment;
-
sexual contact (anal sex, fisting) is rare but particularly higher among MSM, or those with STIs or HIV.
|
| How to Prevent |
-
Practice personal and food hygiene, like you already should be doing. Scrub your hands with soap and wash them before preparing, eating food and after toilet;
-
Drink only boiled or bottled water. All food, especially shellfish such as oysters, clams, etc. should be cleaned and thoroughly cooked before your clam jam.
- Avoid any behaviours that may potentially contact with faeces of other people, and avoid contacting any potentially contaminated objects.
|
-
practice safer sex behavior (wrap up your cock!!!);
-
Don’t share your dildos and other sex toys. If contaminated by blood, the toys should be cleaned with 1:4 diluted household bleach;
-
Never share needles. Use disposable needle and injecting equipment each time (in other words, DON’T DO DRUGS. JUST. DON’T.);
-
Do not share personal care items e.g. razors, toothbrushes, nail cutter etc.
-
Don’t use dirty needles for acupuncture, piercing or tattooing. Those needles and other equipment should be sterile and/or disposable;
-
For HBV infection, if your sexual partner is known to be a carrier, consult your family doctor.
|
| Vaccine |
-
Recommended for men who have sex with men (MSM) with high-risk behaviors such as rimming, unprotective sex and casual sex.
In general, the body takes 2- 4 weeks to develop antibody against hepatitis A infection after vaccination. |
Recommended for all populations, not just the gay community. |
THERE IS NO VACCINE AVAILABLE!!! |
| Treatment |
|
|
-
Consult your family doctor for assessment if you have symptoms of hepatitis;
-
Drugs, such as Interferon, Pegylated Interferon and Ribavirin, can be used to treat the infection. But treatment is not always successful.
|
| Remark: Hepatitis E is also common in Hong Kong. For details, please click Viral Hepatitis Preventive Service website |
 |
1. |
What is HIV and HCV coinfection? |
Ans: |
Co-infection means you have contracted two viruses, HIV and HCV, at the same time。
|
2. |
Is it worse to have HIV and HCV coinfection? |
Ans: |
A person infected with HIV has a lower level of immunity, making it harder for him to clear HCV. Moreover, co-infection with HIV and HCV can lead to more severe disease and faster progression of hepatitis. This seems to be the case even if you have a high CD4 count.
|
3. |
What is the effect of HCV on HIV? |
Ans: |
HCV makes HIV treatment more complicated. Many drugs used in HIV therapy are metabolised by the liver, therefore chronic HCV infection may increase the hepatotoxicity of antiretrovirals.
|
4. |
Should I test for HCV if I am HIV carrier? |
Ans: |
It is recommended that people infected with HIV should have HCV testing regularly.
|
5. |
How long after exposure to HCV does it take to test positive by HCV antibody test? |
Ans: |
HCV infection can be identified by HCV Antibody testing. Usually HCV Ab will be positive 6-8 weeks after exposure, but can be up to 6 months. However, it is important to know that many people who have hepatitis C have no symptoms during acute infection.
|
6. |
Can a person spread Hepatitis C without having symptoms? |
Ans: |
Yes, even if a person with Hepatitis C has no symptoms, he or she can still spread the virus to others.
|
7. |
What are the risk factors for developing chronic HCV infection? |
Ans: |
The risk factors including:
Age at time infection > 25
Male gender
No jaundice and symptoms during acute infection
HIV infection
Immunosuppression
|
|